Entamoeba histolytica
Contributor: Louise Trudel (previously with the Laboratoire de santé publique du Québec)
Biology: Entamoeba histolytica is the only intestinal amoeba pathogenic for humans. It can be found in stool as trophozoites and cysts. Trophozoites are mainly found in liquid or semi-formed stool. Cysts can be present in semi-formed stool, mainly as immature cysts (1 or 2 nuclei) or in formed stool mainly as mature cysts (4 nuclei). Cysts are resistant in the environment, contrary to the trophozoites, and are therefore responsible for transmission of the parasite.
Trophozoites are specifically identified on modified hematoxylin stained smears; cysts can be identified on iodine or modified hematoxylin stained smears. Trophozoites measure usually 15-20 µm (range 10-60 µm) and cysts, about 12-15 µm in average (range 10-20 µm).

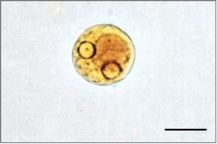
Figure 1. E. histolytica/E. dispar immature cysts with 1and 2 nuclei (iodine staining - 1000X). Source: Laboratoire de santé publique du Québec.
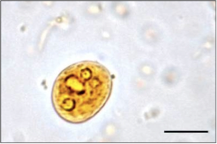
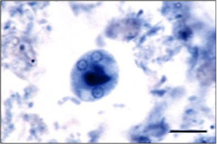
Figure 2. E. histolytica/E. dispar mature cysts with 4 nuclei (iodine/modified hematoxylin staining - 1000X). Source: Laboratoire de santé publique du Québec.
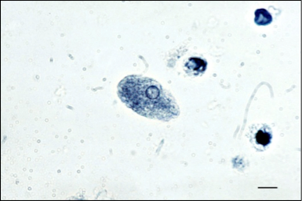
Figure 3. E. histolytica/E. dispar trophozoite (modified hematoxylin staining - 1000X). Source: Laboratoire de santé publique du Québec.
Life Cycle: E. histolytica is transmitted following the ingestion of mature cysts in fecally contaminated food or water, or directly by fecal-oral contact (e.g. contaminated hands, sexual contact). After ingestion, excystation occurs in the small intestine and the trophozoites migrate to the large intestine where they multiply by binary fission. After a while, trophozoites encyst and both stages can be excreted in the stool. When the trophozoites remain in the lumen of the intestine, they usually cause no symptoms. However, they can invade the mucosa of the large intestine, pass in the bloodstream, and disseminate to other organs (e.g. liver, lungs and brain), all of which may lead to the onset of symptoms.
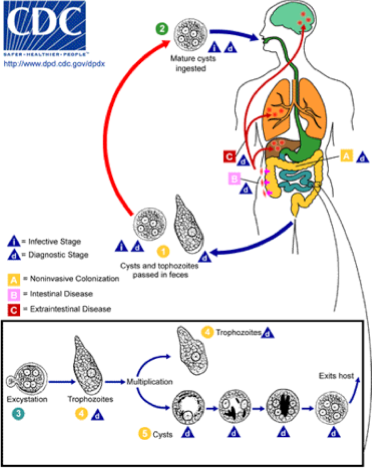
Figure 4. Life cycle of E. histolytica (Source: CDC).
Prevalence: Reported worldwide but more frequent in developing countries. In developed countries, it is usually seen in immigrants, travellers, male homosexuals and institutionalized populations.
Symptoms: Dysentery or bloody diarrhea, fulminating colitis, amebic appendicitis, and ameboema of the colon. In extraintestinal disease, hepatic, pulmonary or rarely brain abscesses as well as cutaneous or genital lesions can occur; no symptoms in carriers. It is estimated that few infected individuals will have invasive disease (2 to 8%).
Laboratory diagnosis: Amebae such as E. histolytica, are usually diagnosed in stool by microscopic examination of permanently stained smears (e.g. hematoxylin) or after concentration on wet mounts, with or without iodine stain. It can also be identified in aspirates or biopsy samples obtained during colonoscopy or surgery.
However, E. histolytica is morphologically identical to Entamoeba dispar, which is nonpathogenic. Therefore, differentiation cannot be made on the basis of microscopical examination (unless red blood cells are found ingested in the trophozoites of E. histolytica, which is rarely seen). Following microscopy, the result is then reported as E. histolytica/E. dispar.
At the Laboratoire de santé publique du Québec (LSPQ), we developed a PCR technique enabling us to differentiate E. histolytica and E. dispar. However, this molecular method cannot be used on SAF- or formalin-fixed specimens received for diagnosis of intestinal parasites. Therefore, when the complex E. histolytica/E. dispar is identified, a new stool specimen is requested with a portion unfixed and frozen as soon as possible. The unfixed specimen must be sent on dry ice to the LSPQ to assure ideal conditions for analysis. With this method, the differentiation between both species can be done.
E. histolytica is rarely identified in those specimens. An average of only 6% of the positive specimens (range 2.4 to 9.5% in the last 10 years) received for differentiation at the LSPQ were identified as E. histolytica, which is consistent with the data reported above. Usually, it is recovered from immigrants or travellers to endemic areas. Differentiation is therefore useful to avoid unnecessary treatment for patients infected with E. dispar.
Antigen detection can also be used to differentiate E. histolytica from E. dispar. A few EIA commercial tests are available that can identify E. histolytica specifically; however these tests can be performed only on fresh or frozen stool (as for PCR testing). Serodiagnosis (e.g. EIA) is also available. Sera are positive only in invasive disease. However, antibodies can persist in the blood for many years; so a positive result is not necessarily indicative of an acute disease. Serologic analyses are available at the National Centre for Parasitology, Montreal General Hospital, in Canada.
Treatment: Iodoquinol, paromomycin or diloxanide furoate (not available commercially in the U. S.) for asymptomatic patients; metronidazole or tinidazole, followed by iodoquinol or paromomycin for mild to severe intestinal disease and extraintestinal disease.
Control measures: Improved disposal of feces in developing countries, good hygiene, avoiding ingestion of unboiled tap water when traveling in endemic countries, washing of fruits and vegetables, cooking and freezing of foods are all effective in reducing the risk of contamination.